Washington: The number of veterans who were hospitalised in between 2005 and 2014 required amputation or died due to critical blockages in their leg arteries decline, said a recent study.
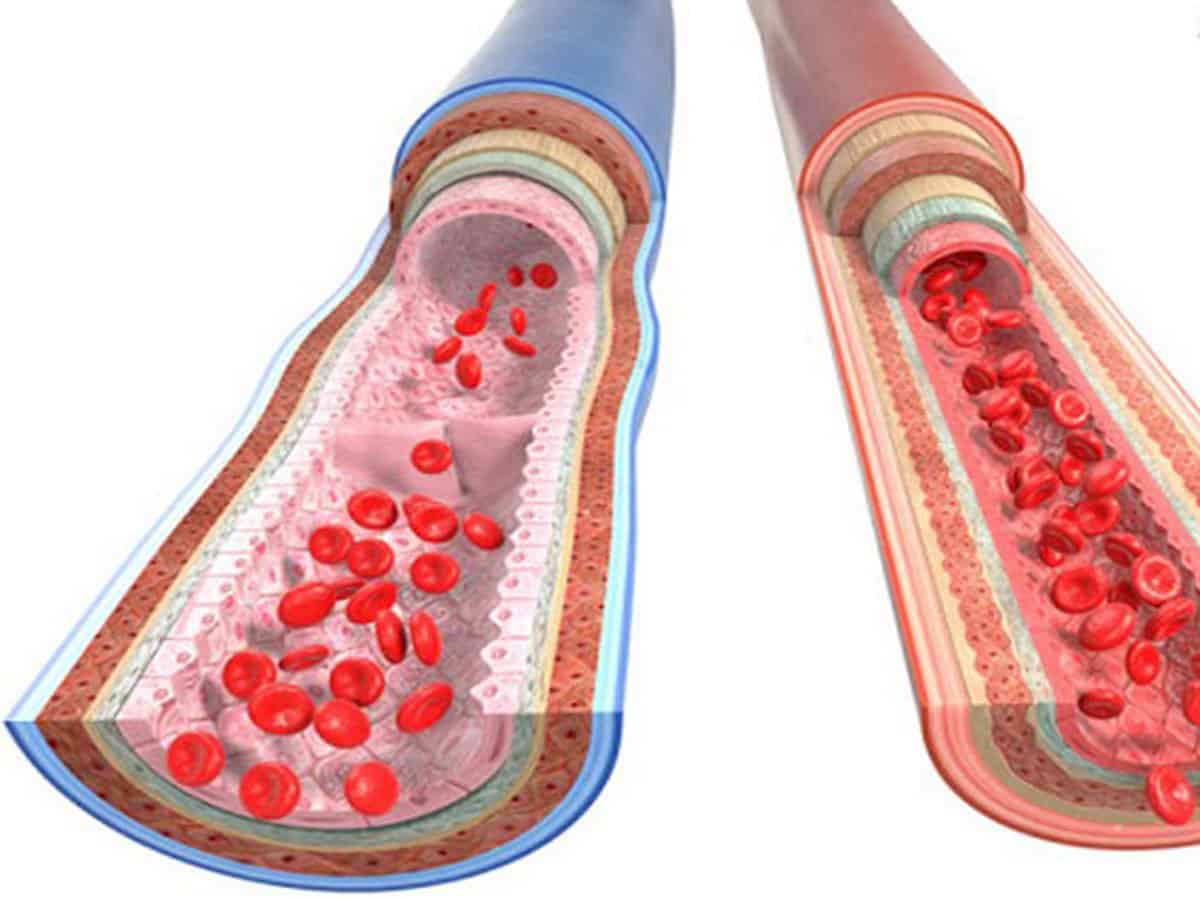
Critical narrowing of leg arteries — called critical limb ischemia (CLI) — is an advanced state of disease in arteries that can lead to severe leg pain even at rest, wounds that don’t heal and a very poor quality of life.
Without proper treatment, CLI can lead to amputation, which further decreases mobility for daily living and severely impacts the quality of life. Patients with CLI are also at high risk to have a heart attack or stroke.
The study was published in the journal of ‘Circulation: Cardiovascular Interventions.’
The improvements in patient outcomes paralleled an increase in the number of veterans with CLI who underwent procedures to restore blood flow, either via surgical bypass or a less-invasive endovascular procedure to insert a stent to hold the artery open. These revascularisation procedures can be effective in alleviating pain, improving wound healing and avoiding amputation.
In this retrospective analysis, researchers found overall positive trends among veterans treated for CLI at Veterans Affairs (VA) medical centers, yet there were potential areas for improvement. Many veterans were not taking recommended statin medications, and almost half of those who underwent amputation did not first receive a procedure to try to restore blood flow to the impacted limb.
“All patients with CLI should be evaluated to determine if they could benefit from a procedure to restore blood flow,” said Saket Girotra, MD, SM, senior author of the study and assistant professor of cardiovascular medicine at the University of Iowa Carver College of Medicine in Iowa City.
“In addition, patients with CLI should be aggressively treated with medications, including statins, blood pressure medications if they are hypertensive, and drugs to reduce platelet stickiness in order to reduce the risk of heart attack and stroke.”
To identify trends in treatments and outcomes, the researchers examined nationwide data from all VA facilities for nearly 21,000 patients (average age 68) who were hospitalized for CLI between 2005 and 2014.
Researchers found that mortality decreased from 12 per cent to 10 percent (after adjusting for other risk factors). Amputation decreased from 20 per cent to 13 percent (after adjusting for other risk factors). The patients who underwent procedures to restore blood flow were 55 percent less likely to die and 77 percent less likely to undergo amputation.
There were sharp differences among VA hospitals in the proportion of patients receiving revascularization procedures, ranging from 13 per cent to 53 per cent, with little of the variation easily explained by differences in patients.
Although the researchers had access to information on patients’ other medical conditions that might influence the decision to undergo an invasive procedure, they did not have information on the extent of disease in the arteries.
“The disease may have been too advanced in some patients, making surgery or stenting not feasible, therefore, the only option was an amputation to limit the spread of infection and gangrene. A more in-depth study is needed to determine if revascularization was not offered to some patients who may have benefited,” Girotra said.