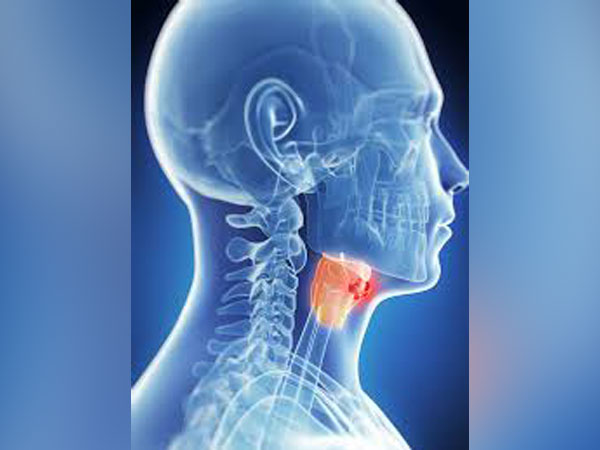
Washington: A new technique that illuminates blood flow during surgery that can predict complications and enables surgeons to make adjustments during larynx cancer surgery or recovery to improve outcomes.
The study was published in the journal ‘Annals of Surgical Oncology’.
“Radiation damage is something you can’t always see. There have been very few examples in the literature that would explain or predict who’s going to have a complication,” said Matthew E Spector, senior author of the study.
Researchers enrolled 41 patients who were undergoing laryngectomy after radiation.
After removing the tumour but before closing the throat, anesthesiologists gave the patients an intravenous injection of a type of medical dye, indocyanine green.
The dye circulates within about 40 seconds. Surgeons then use laser angiography, which illuminates the dye, allowing them to observe blood flow.
The results were clear-cut: patients with lower blood flow had a significantly higher risk of developing a fistula, whereas patients with high blood flow had a very low risk of wound complications.
Knowing this, Spector suggested a few possible interventions.
One could be cutting out a wider margin of tissue to get a cleaner, healthier edge. Another possibility is to keep high-risk patients in the hospital longer while sending the low-risk patients home more quickly.
Most people with larynx cancer will have radiation and chemotherapy. But about one-third of the time, cancer will return or will prove resistant, leaving surgery as the next option.
At this point, tissue damage from the radiation adds challenges to the operation. When the surgeon closes the wound, damaged tissue can interfere.
For about 40 per cent of patients, this will lead to a pharyngocutaneous fistula, a hole in the neck where saliva can leak out.
It can cause bleeding or infections, keeping patients in the hospital longer and in 10 per cent of cases sending them back to the operating room to fix it.
It’s already used by other surgeons, including in breast reconstruction. Many hospitals already own the equipment.
[source_without_link]ANI[/source_without_link]