Washington D.C. [USA]: A group of researchers from Canada has developed a ‘handheld 3D printer’ that has the ability to print new skin cells on severe burn injuries that are too extensive to be treated with conventional skin grafting.
The prototype of the device has been successfully tested and the results of the experiment were recently reported in the IOP publishing journal Biofabrication.
Senior author and professor Axel Gunther, from the University of Toronto, said: “Skin grafts, where the damaged tissue is removed and replaced with skin taken from another area of the patient’s body, are a standard treatment for serious burns.”
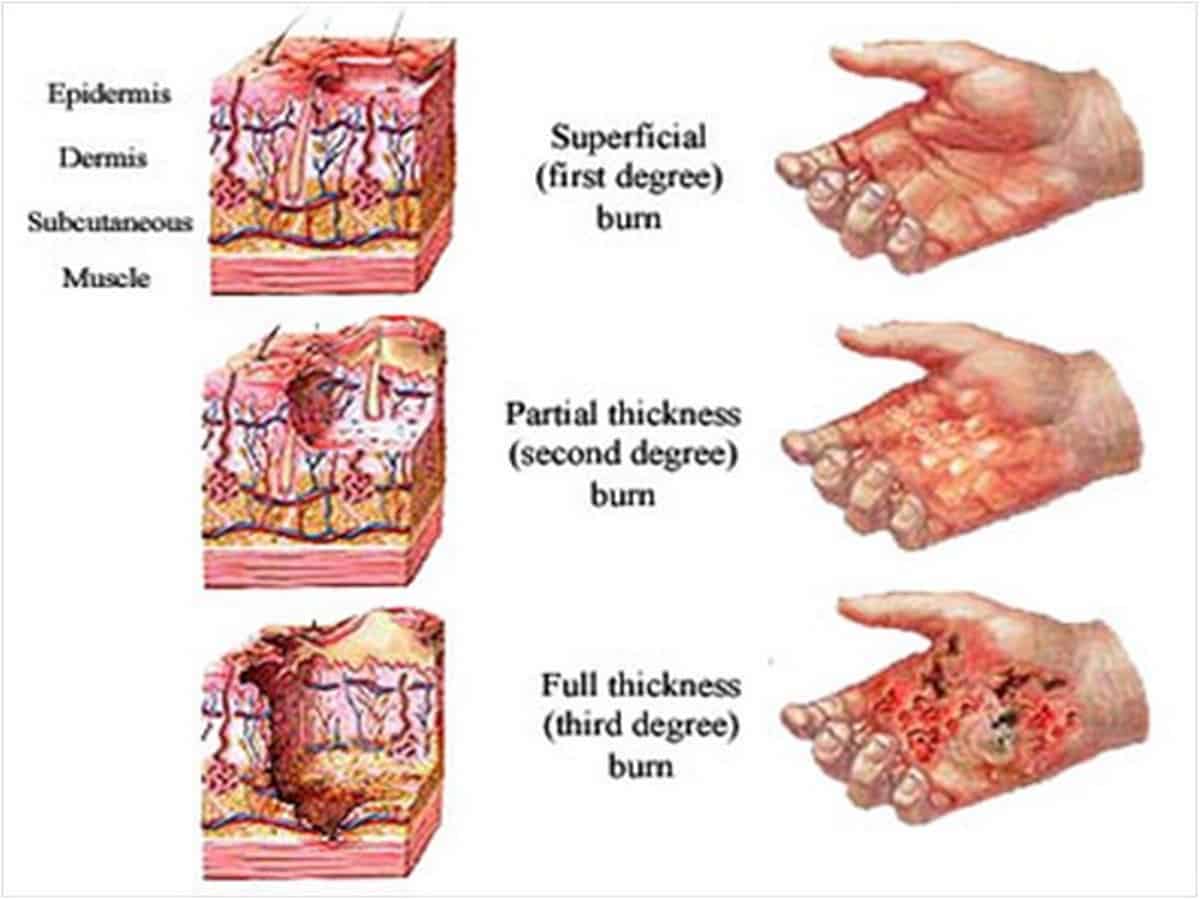
“However, in cases where a patient has extensive full-thickness burns — which destroy both the upper and lower layers of the skin– there is not always sufficient healthy skin left to use,” Axel added.
The senior author also shared that while there are alternatives including scaffolds using bovine collagen or engineered skin substitutes grown in vitro, none is ideal.
To overcome these challenges, the research team designed the handheld device to deposit precursor sheets directly onto wounds of any size, shape or topography.
Co-author Dr Marc Jeschke, medical director of the Ross Tilley Burn Centre at Sunnybrook Health Sciences Centre in Toronto, said: “In general, the wound surfaces we designed this device for are not flat, nor are they oriented horizontally. One of the most important advantages of the device is that it should allow for the uniform deposition of a bioink layer onto inclined surfaces.”
Marc continued saying that in this study, “we tested whether the device could do this effectively by using it to treat full-thickness burns in pigs. We found the device successfully deposited the ‘skin sheets’ onto the wounds uniformly, safely and reliably, and the sheets stayed in place with only very minimal movement.”
“Most significantly, our results showed that the MSC-treated wounds healed extremely well, with a reduction in inflammation, scarring, and contraction compared with both the untreated wounds and those treated with a collagen scaffold,” the co-author opined.